letters to little liberte: 03
/hi adeline,
This is the very first picture of you. Daddy took it. I hadn’t even seen you yet — the NICU team had to take you right away to make sure you were given the immediate care you needed.
You were born on April 26, 2023 at 6:46 p.m. You weighed just 4lbs 5.6oz. You weren’t supposed to come for 10 more weeks.
Dubbed our sunshine girl, you were born on the first 70-degree day we had since last October.
I wasn’t sure when I’d be ready to write your birth story — and to be honest, I’m not sure I’m ready now —, but I still remember it like it was yesterday and I don’t want to wait too long for fear that pieces of our incredible story will start slipping from my memory.
And you know what’s interesting about my decision to write this now? I looked at the calendar and it just so happens that Wednesday this week (in two days) marks 30 weeks out of the womb for you. You only got to be cozy and growing in there for 30 weeks and now you’ve been out for 30 weeks. What odd (and serendipitous) timing.
You’re almost 30 weeks old but you’re supposed to only be 20 weeks old. There’s a constant math equation in our heads when we think about your milestones and development. Having a preemie isn’t as easy as “oh she’s 6 months old so she can now ____”; we are always subtracting time from your age to make sense of where you’re at and how you’re developing.
For the record, you’re perfect.
Picture 1 was taken November 3rd, 2022 at 5 weeks pregnant. Picture 2 was taken January 29th, 2023 at 18 weeks pregnant. Picture 3 was taken the day you came, April 26th, 2023 at 30 weeks pregnant.
I share these pictures to show how my severe preeclampsia progressed. Of course, we didn’t know I had it until 25 weeks gestation when I was diagnosed and hospitalized, but once we were in the hospital it was tough to understand just how swollen I had become due to the disease. When you’re in it daily, you don’t see it. While there were so many other “invisible” symptoms to the outside eye, this was the most “obvious” symptom — and what’s hard, especially as a first-time mom, is that I just thought the swelling I had was a “normal pregnancy thing.” I’ll save everyone the pictures of my excessively swollen feet, but let’s just say — it was scary and totally not normal.
I started taking daily face pictures in the hospital when one of my favorite OBGYN doctors came in to talk to us one morning when my labs had taken a turn for the worse. She kindly said: “I’m not being mean, but you look puffier than normal. Pay attention to your face swelling because I don’t think you looked like this even a week ago.” She also told us that morning — as gently as possible — that she would be surprised if we made it through that week. I was devastated.
We kept having conversations with doctors and nurses about the growth and development milestones you were having each week while still in the womb. Our ultimate goal was to get you to 34 or 35 weeks — coming to terms with you likely arriving more than a month earlier than that felt impossible, especially when we kept hearing even 32 weeks was such an important goal.
The main concern for all of us was your lung development. When I was first admitted and things were quite scary and they weren’t sure how or if I would respond to the medication, they gave me a steroid shot to help your lungs develop quicker. But it only helps for 2 weeks and it had been almost 5 weeks since they gave it. They can also only give it twice. So we asked that same OBGYN what she would do if she were in our situation given my labs going in a downward spiral. She said she would get another steroid shot — so we did.
And thank god we did because you came only 4 days later.
your birthday
When I woke up, the first thing I told the on-site doctor that day (the doctor who delivered you, Dr. Barrett!) was that I felt like I was getting sick — like that shaky, weak feeling you get when you’re coming down with a cold or flu. I remember she put on a mask after I said this (just in case) and told me that she remembered feeling like this toward the end of her pregnancy when she had preeclampsia with her first — that the combination of everything my body was going through with pregnancy, severe preeclampsia, and gestational diabetes in addition to the cocktail of meds I was on (7 different medications: nifedipine and labetalol 2x per day to control blood pressure, insulin 4x per day plus more as needed to control blood sugar, protonix 1x per day to help with crushing epigastric pain, and my other normal vitamins and medications 1x per day) could really wear down my system.
I went on with my normal morning routine, constantly thinking about how much you were (or weren’t) moving. Your movements had significantly slowed down since the weekend prior and I had been keeping my medical team updated because I was quite concerned. A normal day consisted of 2x monitoring you — once in the morning and once in the evening — unless you weren’t meeting the accelerations and decelerations they needed to see. You were always hard to monitor — a little wiggle worm — but over the last several days we had to do additional BPP monitoring with an ultrasound because you weren’t showing us you were stable in there with just the heart rate monitor.
The day before you came, one of my nurses came in to stop me from eating breakfast “just in case” we had to do a c-section that day given all of our monitoring concerns. But… I woke up starving and had already eaten a bar that morning. So she let me eat breakfast and we thankfully didn’t have to deliver that day.
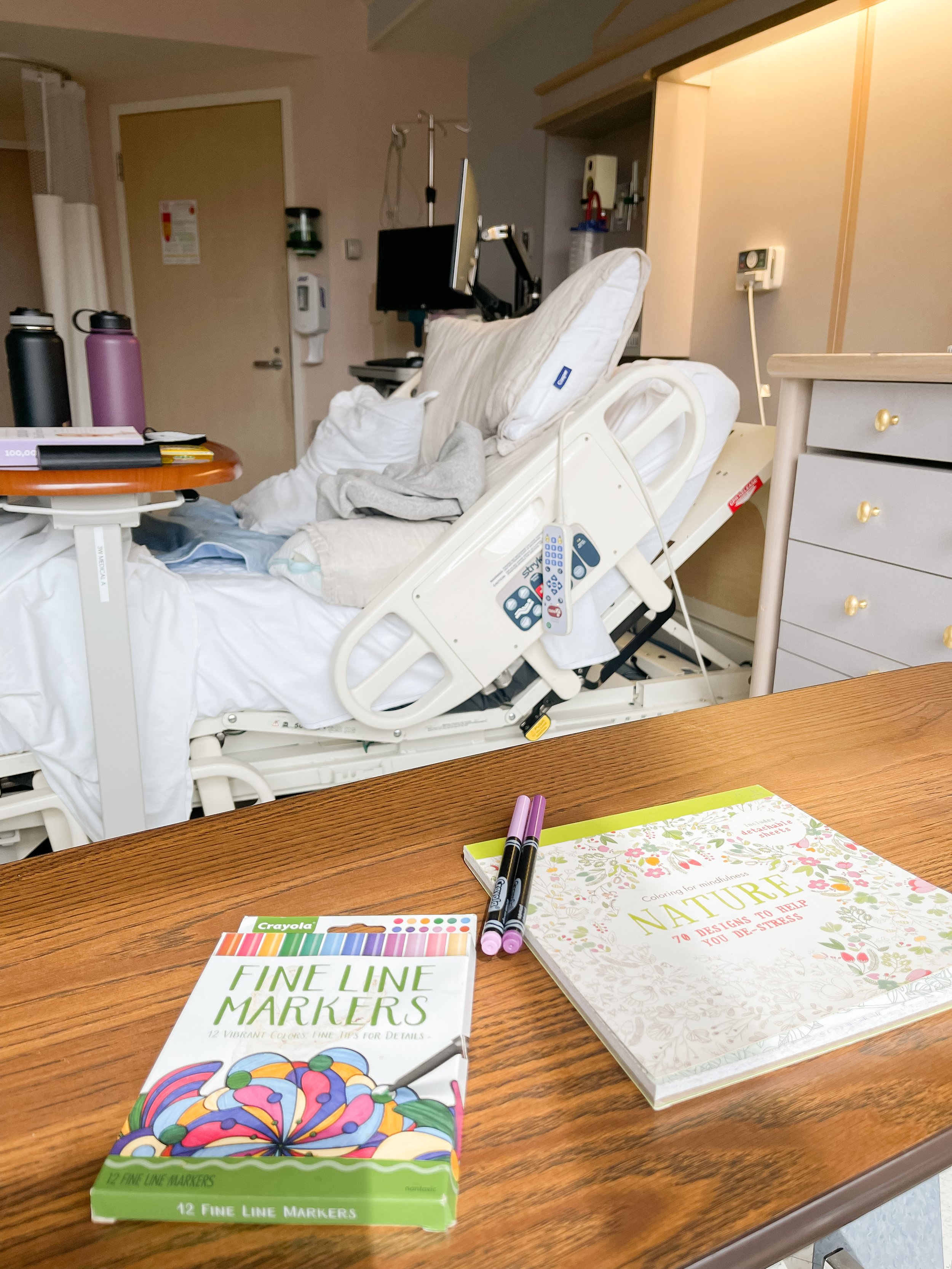
On your birthday, I got up, washed my face, put on some clothes, and ate breakfast. I was so tired. We hooked you up to the heart monitor and I put on some shows and movies on my computer. I was falling in and out of sleep and just remembered feeling absolutely drained and exhausted. We weren’t seeing what we needed to see from you and we had already done 3 BPPs in the days leading up to this day. The nurse told me a fetal monitoring specialist was going to come to speak with me; she said that what she was seeing wasn’t super reassuring and I would need to stay on the monitor until we saw what we needed to see — or until we had to make a call to deliver.
Although I was so upset leading up to that day because everything was pointing in the direction of a very early delivery, a sense of peace came over me after speaking with the specialist. I was simultaneously absolutely terrified and mad at my body for failing us AND I knew that it had worked so hard to get this far and didn’t have any fight left in it.
About halfway through the day, the nurse came in and brought the c-section prep kit and let me know they were cutting off my food intake “just in case.” I called everyone to let them know, including daddy who was on a work trip to Home Depot looking at the cost of building materials 😂
The specialist came in shortly after and still didn’t have a firm decision. So I laid there falling in and out of sleep as they continued to monitor you. Daddy came to the hospital as soon as he was off work and shortly after, about 5pm or so, Dr. Barrett, the specialist, and a handful of labor and delivery nurses came rushing into the room.
The decision was made. You had declared yourself and were coming this evening.
So they started me on a magnesium drip to help prevent strokes and seizures during and after delivery and got everything else prepped. I remember getting emotional as everyone was rushing around and telling daddy and I things about what to expect.
Finally, they wheeled me back to the operating room.
The anesthesiologist started the spinal tap, which is normally a very quick, easy thing, and I kept feeling the needle — meaning it wasn’t quite getting into the right spot. I vividly remember Dr. Barrett standing in front of me looking me in the eyes and holding my hands, reassuring me the whole way through. She made me feel safe, even through my tears.
The team asked me a few times for my name and birthday and read aloud my blood type, to which Dr. Barrett exclaimed, “hey, that’s my birthday and blood type too! It’s meant to be that I’m on call today!” 🤗
The spinal tap still wasn’t working and Dr. Barrett noticed I was going pale white, so they laid me down and tried to do it that way. They sent a nurse out of the room into the hallway — where daddy was waiting — to get a cold wash cloth for my forehead.
Finally, they got the spinal tap to work and I felt an immediate rush of tingles all the way down my body. They laid me down and asked me if I could still feel anything in my torso area and I touched on my left side where I could feel, forcing them to re-sterilize that area (oops 🤪). After a few minutes, everything was numb and daddy was finally able to come in the room.
The c-section simultaneously felt like a blur and like it lasted forever. I mainly remember this odd feeling of tugging throughout the surgery, as well as feeling totally nauseous on and off. The anesthesiologist would give me something every time I felt nauseous that made me feel better — but he also gave daddy a puke bag just in case. The lights on the ceiling were kind of mirrored so I could see the surgeons’ hands working, but not the detail of it.
When they finally delivered you, you let out a tiny cry and my eyes welled up — it was such a good sign that you cried. It meant your lungs were working in at least some capacity. I looked at daddy and said “it’s good, the baby cried” as the NICU team whisked you away.
The surgeons asked daddy if he wanted to announce girl or boy, but neither of us had seen you! Finally, someone said “it’s a girl!” and I remember saying so many times how I couldn’t believe I was right — I had an intuition from early on in our pregnancy you were a girl. What an amazing moment.
We didn’t get our golden hour and I didn’t even get to see you until several hours later, but your birth was still magical. Daddy and I were so happy and relieved that you were here. We were also scared for what your healing journey — and mine — would be like, but we knew we could tackle it together.
When we finally got to go back to the NICU, they had you in your little incubator, on CPAP, and all hooked up to so many monitors. I remember being so nervous to touch you — I didn’t want to do anything that could hurt your fragile, tiny little body.
But I was finally able to touch your little toes and it was the best feeling — you were real and you were really here. I don’t remember how long we were able to stay in the NICU that night, but it wasn’t long enough.
We had a long journey ahead of us, but we would do it as a family. Daddy and I would fight fiercely for you every day during your 7-week NICU stay — but that’s for another blog post and another day.